Frequently Asked Questions About General IOP

I’ve never heard of an IOP before. Does this sort of thing actually work?
Our program is grounded in evidence-based, third wave behavior therapies with documented effectiveness in treating a range of psychological concerns. A vast body of research confirms that treatment in mid-level care settings like IOPs can significantly improve symptoms such as anxiety and depression, as well as your ability to engage fully in work, hobbies, and time with your family. This effect is achieved through a combination of individual sessions and group therapy, and work together to help you approach your experiences in a different way. Unlike many other private practices, the SCP IOP treatment group is also actively engaged in both reviewing and generating research improving treatment and diagnosis. We place a high value in understanding how and why effective treatment works so we can provide you with the best possible care in our programs.
When does the program day start/end?
You will need to check in daily by responding to an emailed prompt every morning by 8:45AM. Please call the front desk to check in by 8:45AM if you are unable to respond to the emailed form or do not receive it. This lets the IOP team know to expect you for treatment every day, and to plan content and groups accordingly. Patients who do not check in on time may not be admitted to groups or sessions for the program day. The first group starts at 9am and the final group ends at 12pm, though you may have an individual session after the last group.
How long will I be in the program?
Length of stay varies depending on individual needs. On average, most people are in the program for 3-6 weeks.
Will my insurance cover this?
SCP will coordinate with your insurance company to ensure your care is covered. In the event you do not have coverage this will be communicated to you as soon as possible. Deductible and out of pocket costs vary by insurance companies and your specific policy. If you have concerns about your coverage we recommend you speak with your insurance company directly prior to enrolling (be sure to write down what they say, the date/time, and the name of the person you speak with).
How often will I see my doctors?
You will meet with your psychiatrist on your first program day, and with your psychologist or therapist on either the first or second program day. Our intention is that you will have an individual session with at least one provider on most days.
How will I know if my individual team wants to meet with me?
All IOP participants are required to provide an active email address and phone number that is accessible to them throughout their admission. Your team may use either/both of these methods to contact you for individual sessions. Let your team know if you have a preferred method of contact (email vs phone call vs text). Please keep this in mind and make sure you are checking your email and phone regularly during the treatment day.
How can I contact my team if they haven’t reached out to me?
Call the front desk at 401-500-0424 and ask to speak with your team or leave a message for them if they are unavailable. Please do not use Tebra messaging to contact your treatment team for anything that is time-sensitive (unless your provider has specifically requested you do so), as these messages are not always delivered to your providers in a timely manner.
What if I have an emergency and need to leave?
Please call the front desk immediately if you need to be absent or leave the program unexpectedly. You may be asked to speak with an individual provider prior to checking out for the treatment day.
What if I have an appointment I can’t reschedule that interferes with IOP hours (or need to arrive late/leave early for another reason)?
Please make every effort to schedule and reschedule outside appointments to accommodate IOP hours. Let your team know in advance if you have critical appointments that cannot be rescheduled. Depending on the amount of treatment you will miss, you may need to cancel a day or days of IOP, or reschedule your start/discharge dates from the program. Repeated missed sessions for any reason may result in discharge from the program, so it is important you coordinate closely with your individual team about any planned absences.
My childcare fell through today (or my infant is very young), can I log in anyway and just do my best?
We are genuinely sympathetic to the demands of daily life, particularly childcare limitations. Even so, it is difficult to split attention between two very important tasks (childcare and treatment). There are frequently topics, stories, or other specifics happening in groups that would not be appropriate for a child to overhear. It is our experience that the needs of children requiring supervision significantly limits full participation in group activities. Therefore, the presence of children–even very young children– is prohibited during treatment activities.
Please talk with your treatment team as soon as possible if you anticipate childcare demands may limit your participation in the program, and we will do our best to discuss options that may be available to you.
I can’t attend groups but I need to talk to my doctor(s). Can I just do my individual appointments today?
Unfortunately IOP is structured, scheduled, and billed as a comprehensive program. In most cases it is not possible to see your individual providers if you are not checked in for the full program day. Please reach out to the front desk if you have questions about your individual care or need to connect with your doctors directly on days you are not in attendance at IOP. If you are not in attendance assume any prescheduled individual appointments with your IOP providers are canceled until you return.
Who is allowed to be in my sessions? Can I ask my partner/friend/family to attend with me?
We absolutely recognize and honor the importance of your close relationships to your mental health and well-being. Typically your sessions will start with just you and your doctor(s). After that, additional sessions may include others at your and your doctor(s)’ recommendation. Please communicate directly with your team about anyone you would like to include in your care, and we can discuss and plan thoughtfully how to integrate them as it benefits your individual treatment plan. Please note that for confidentiality reasons we cannot include anyone other than enrolled patients in group sessions.
What kind of trainees will I encounter at SCP IOP?
Providing exceptional training in mental health is integral to our mission at SCP. Having more providers who understand mental health improves your experience in the wider community, and hopefully leads to more sensitive, informed, and supportive treatment options nationwide.
You may encounter trainees from a variety of professions during your admission, including doctoral psychology externs or fellows, psychiatry residents or fellows, masters level therapists, nurse practitioners seeking psychiatric training, medical students, and/or other advanced practitioners. Please know you always have a right to know who is in the room with you, their name, and their reason for being present, as well as the right to decline having trainees in your individual sessions. Trainees operate under our licenses and are subject to the same laws and professional standards governing privacy as your other doctors. Talk with your individual treatment team if you have any concerns about having trainees present as part of your treatment.
I need paperwork to be out for TDI/work/school/etc. Can IOP provide this? What about help with SSDI?
We are happy to provide documentation of your participation in the program and dates of admission to work, school or any other relevant parties provided you sign a release for us to do so. Often we can also help with TDI paperwork, though this will depend on your specific case. Due to the short duration of the program we typically do not provide support or help for SSDI or long-term disability cases.
I need help with social services (for example, food stamps, paying bills, legal advice, housing). Can SCP help me with that?
Unfortunately we do not currently have a social services clinician on staff at SCP.
Will my IOP team talk to my outpatient doctors?
We at SCP are committed to setting the standard for excellent and coordinated care for everyone in our programs. Part of providing good care is working effectively with your outpatient team. At intake you will be asked to provide a release of information for us to speak with each member of your outpatient mental health team, typically your individual therapist, psychiatric prescriber, and primary care doctor. We will then make outreach calls to inform them of your admission and to discuss any pertinent information to provide the best possible support while you are in IOP. After you discharge from the program we will send a brief discharge summary detailing the treatment provided as well as any recommendations for your care moving forward.
Can I still see my outpatient therapist and psychiatrist while I’m in the IOP?
We generally do not recommend seeing your outpatient providers while you are enrolled with us. IOP level care can be both emotionally exhausting and time consuming. Hearing feedback from different sources can also be confusing and make it harder for you to benefit fully from treatment in our setting. Importantly, insurance companies often will not cover outside individual sessions in addition to IOP. Please coordinate first with your IOP treatment team if you plan to see any outpatient mental health providers while you are enrolled in the program.
What if I don’t have an outpatient team, or don’t like the one I have? Will SCP help me find new providers?
It is the policy of the SCP IOP not to provide referrals for outpatient providers if you already have an outpatient team. Changes to your outpatient team should be coordinated directly with those individuals and not done in a short-term setting such as IOP.
If you do not already have providers for therapy and psychiatric medication– and IOP recommends you have those providers– we will do our best to provide resources and suggestions to support you establishing care with outpatient providers in the community. Please note that we do not currently have a discharge planner on staff, and you will be expected to make your own phone calls and appointments.
Can I change individual providers at IOP if I don’t like my team?
It is the policy of the SCP not to change individual treatment team assignments. Concerns about your treatment team should be brought up directly with those individuals, openly, genuinely, and with a spirit of willingness to find middle ground to address problems in your care. Skills and process group discussions can provide support for these discussions as well.
My individual provider is out today, what does this mean for me?
We make every effort to ensure that your individual needs are met. That said, sometimes illness and other unplanned events keep us away. The larger IOP treatment team will make every effort to ensure your needs are met regardless of the presence of any specific individuals. Please let us know via the front desk if you have any needs in the absence of your individual team member(s).
I really like my team and want to keep them! Do IOP providers see outpatients?
Thank you, we like seeing you too! Most of our IOP team do not have openings for individual outpatients, however it never hurts to ask. You should ask your doctors directly if this is of interest to you. At a minimum, we may be able to guide you in finding providers who are similar to us in their approach and training. Please keep in mind that as a matter of SCP policy we will not transfer care or refer out if you already have an outpatient team.
Can I talk about triggering things in group? What is off-limits?
People come to SCP IOP for a variety of reasons, and it is common for these stories to include things that others consider upsetting. These experiences are both important and treatment relevant, and you should anticipate they may come up in a general way in your groups. For example, in groups we may reference having a history of trauma, self harm, substance use, legal problems, and grief or loss among other things. This is particularly true in process group, where the discussion is less structured and people may be practicing skillful ways of communicating about very painful experiences. It is also reasonable for you to talk about and receive support for your experience hearing these stories.
That said, detailed discussions of trauma, violence, substance or alcohol use, self-harm, suicidal thoughts or urges, and other difficult experiences may not be appropriate for groups. This is particularly true for stories or comments that glorify, make light of, or otherwise misrepresent the seriousness of these events. Keep in mind that we expect you to bring content to group that you are ready and willing to engage with feedback and work actively on. If you are unsure whether or how to talk about your experiences please check with your group leader or individual providers.
I have to be away for a day (or days), but I don’t want to miss treatment. Is it okay if I log in from somewhere else?
For safety reasons it is required that you provide an accurate, physical location from which you plan to log in daily. Should anything happen requiring support we need to know where you are! Changes to your physical location should be reported on the daily check in form, or you can call the front desk directly at 401-500-0424.
That said, there are strict licensing regulations that limit where our providers can provide treatment. Regulations and licensing can change, so please contact the front desk if you have any questions about where you can be located to receive treatment through our IOP.
What is allowed on camera?
The SCP IOP takes place entirely in a virtual setting, which means that every day we are present with you in your home or other personal space. Generally speaking, we ask you to (1) minimize distractions during group and (2) be thoughtful about what is visible on screen in your home. Try to minimize movement and other activities such as eating, walking, or taking phone calls during group times. Substance and alcohol use–including vaping and/or taking medication– is specifically prohibited on screen during group time. Importantly, things such as drug paraphernalia, strong political statements, art displaying expletives, or other potentially triggering content/items may be distracting or problematic in group treatment. Please ask your individual treatment team if you are unsure about whether any items or activities are appropriate on screen during your groups.
I will be driving home but don’t want to miss any of my sessions! Can I log in and just listen?
We are glad you don’t want to miss any part of the program. We don’t want you to miss your sessions either! That said, we also want you to be able to give your full attention to the treatment you are receiving, and to be safe and private while doing so. For these reasons, driving or being a passenger in a moving car during any program activities is strictly prohibited. If you are observed to be driving during any part of your treatment you will be removed from the session and asked to return as soon as you have reached your destination safely.
I’m really tired but I don’t want to miss my groups. Can I keep my camera off in groups? Can I be in bed but still listening?
Groups are the backbone of IOP care, and we are glad when these questions arise because it suggests you are thinking seriously about how to get the most out of your group time! As a general rule, we request that you present to groups sitting upright, with your eyes on the screen/other group members, and minimizing distractions. Come prepared to participate actively including putting your best effort into guided activities, sharing your experiences, and supporting others. For privacy reasons, you must have your camera on and be visible on screen for the duration of the group. Please let your individual team know as soon as possible if you anticipate any difficulties being able to engage with groups in the manner described, and we will problem solve together in a way that best meets your and the groups’ needs. You may also contact the front desk directly if you have any immediate questions about group behavior and what is workable for you. It is also fine to ask the group leader if you have any questions about expectations for that particular group.
Group has been really hard for me today! Is it okay to take a break?
Groups are an important part of your IOP care and can be emotionally intense. If you are noticing feeling emotional in a process group the first step is often to let the group know, as group reactions are a common part of the discussion. It is much preferable to remain in the process group and get support versus being alone with any reaction.
That said, if you are in a skills group, don’t feel it is appropriate to share your experiences, or feel too overwhelmed to communicate with the group about your emotions, it is absolutely fine to take a brief break. Breaks from a group can be an opportunity to practice skills learnt in the program, and to share that practice with your groups/team at a later time. However, we do request you keep breaks as brief with a quick return to the group if possible. Frequently missing groups or even portions of groups may negatively affect your treatment and should be discussed with your treatment team.
What if I’m too upset to come to group at all?
As we’ve noted, the program is designed to work best as a complete package, and it is critically important that you attend all sessions as scheduled. Indeed, many of our sessions are specifically designed to help you in moments when you are most upset! We are best able to help you if you attend the program and we are aware of what is happening, so please absolutely attend all sessions, especially if you are feeling distressed or unmotivated.
Help I can’t get into my group or it keeps logging me off!
Please contact the front desk immediately if you have any difficulty accessing or staying logged into your groups. Often our front desk staff is able to troubleshoot basic issues affecting group access, or provide feedback for why your groups are being logged off. You may wish to have a family member or close friend available on your first day if you are someone who struggles with technology. Please do not use old links to access your groups unless you are directly instructed to do so.
I want to help someone I met in group. Can I give them contact information for my therapist (psychiatrist, support group, etc)?
Although we do not prohibit it, please be extraordinarily careful with offering or accepting any outside resources or recommendations from other patients. There may be very important reasons your team has not suggested a particular resource to you, and what works for one person may not be appropriate for another. Ask your individual team if you have any questions about sharing or accepting resources from another person in the program.
I know someone in my groups outside of the program! What should I do?
Rhode Island can be a very small community, and it is not uncommon to recognize someone from your groups as someone you also know outside of treatment. Please bring any outside relationships to the attention of your treatment team as soon as you become aware of them, and we will work with you to determine appropriate next steps.
I really connect with someone in my group. Is it okay if I give them my email address/phone number/social media account/etc?
It’s natural to feel caring and connection for other people you meet in IOP, particularly given the emotional intensity that passes within groups daily. This is part of being human! Nonetheless, it is important that you approach these relationships as meaningful and time-limited interactions, and not as a source of long-term support.
We strongly discourage any contact between group members other than in our structured treatment setting. This includes (but is not limited to): exchanging phone numbers, texting/chatting, connecting via social media, initiating friendships, dating/sexual/romantic relationships, networking for business purposes, or any other contact between patients currently in treatment outside of IOP hours. Outside relationships can be problematic for treatment and for your safety. We take both treatment and safety very seriously. Violating this rule may be grounds for discharge from the program.
I really don’t like a person in (or running) my groups. What should I do?
It is both human and expected that you will have all kinds of reactions to people you meet in IOP, both positive and negative. We absolutely expect some providers and group members will be a more natural fit than others! That said, it is important to find a way to minimize the impact of your personal feelings on your treatment. Unfortunately, it is not possible for us to change group or treatment team members as part of IOP.
Please bring it to the attention of your individual treatment team if you are noticing a strong reaction to any individual group leader or member, particularly if that reaction is negatively affecting your care. They will be able to help guide you in using skills and groups to address any interpersonal conflicts if needed. If necessary, they can also coordinate with the entire IOP team to intervene effectively on your behalf.
I don’t like groups (or individual sessions), or I don’t think they help me. Can I just skip them?
It is a requirement of IOP admission that you attend all scheduled/invited group and individual sessions daily. The program is designed with an expectation that all individuals enrolled are receiving all components of care to achieve the best possible outcome.
Nonetheless, we understand that not all experiences will feel equally helpful or applicable to your needs. If you are struggling with any individual topic you can absolutely bring questions to both skills and process groups. Your individual team can also help you to get the most from sessions you struggle with. Similarly, individual sessions are an important part of treatment and it is required that you attend these sessions as recommended by your team.
What if I don’t think the program is helping?
Please speak with your individual treatment team about any concerns about your treatment experience. There may be ways to adjust your care to get more from your time with us. Alternatively, if a transfer of care is indicated, your individual team is best situated to make this happen in a smooth and timely manner.
If you have a complaint about your treatment experience, we first recommend you speak with your individual treatment team. If a resolution is not reached, it can then be escalated to the program director & assistant director at your request, and subsequently to the practice director(s). A copy of our grievance policy can be provided at patient request.
What if I want to talk with my IOP doctors after I leave the program?
Unfortunately we are not able to provide additional support, referrals, or treatment after you left the program. After discharging from IOP your care transfers back to your outpatient treatment team. If you think you need to return to IOP please coordinate a re-referral through one of your outpatient providers.
What if I want to come back after I’ve already completed the program?
People decide to come back to IOP for any number of reasons. For example, new symptoms can arise that we didn’t target in your first admission. Some people find themselves falling back into old patterns over time, and come back for a “refresher” to re-engage with needed skills. Sometimes hard things happen in life, leading to a need for more intensive support again. Finally, some folks are unable to complete the program initially for any number of reasons, and come back to try again when they or their situation has changed. In most cases, when you return we make every effort to place you with your prior IOP treatment team, so you can resume treatment as easily as possible.
If you are unsure about whether or not to come back to IOP, a good start would be to have a frank discussion with your outpatient team about pros and cons of another admission. In some cases the IOP team may have a recommendation to optimize your care, so it can be helpful to have your outpatient doctors coordinate with us when they send in a re-referral.
If you are still unsure about returning to IOP, you may also elect to call the front desk (401-500-0424) to inquire whether it would be possible for you to return. Every case is different, and we endeavor to support you in getting the best treatment fit for your needs.
Who is not a good fit for IOP? When should I look elsewhere?
Broadly speaking, IOP is a good fit for people who (1) have significant mental health symptoms, (2) find those symptoms interfere with their daily lives, and most critically (3) are ready to make changes.
Importantly, IOP providers are not available outside of program hours. If you are unable to stay safe when alone or live in an unsafe/unstable environment, we recommend you seek a higher level of care like inpatient hospitalization. On the other hand, if you are able to find benefit from outpatient services alone you may not need the intensity of IOP treatment.
Additionally, IOP can be time consuming. Our program hours are from 9:00-12:30 M-F. People who are unable to reschedule external commitments such as childcare, school, work, or external medical appointments during this time are not a good fit for IOP treatment.
Our IOP combines the effects of individual therapy, group therapy, and medication management to help you improve your situation. People who are seeking any one of these services alone are not a good fit for IOP. Similarly, if you are only looking for a referral to outpatient providers, IOP is not the right fit for you.
Finally, it is very common for folks struggling with mental health to also struggle with addiction to alcohol and/or substances. If this is you please know first and foremost that you are not alone! If your substance use gets in the way of you being able to get the most out of the IOP (e.g. not being able to maintain sobriety during/after program hours, missing program due to withdrawal symptoms) and/or requires a higher level of care to manage health concerns (e.g., inpatient detox), we will likely recommend you first address your addiction, and then if needed return to IOP to address mental health more directly. Your treatment team can provide resources for programs that specialize in treatment substance use disorders, if that is our recommendation.
What if I have an emergency while I am in the program?
Please call the front desk at 401-500-0424 if you need assistance during program hours. Although your psychologist and psychiatrist may not be immediately available, we will pass along messages and they will get back to you as soon as they can. Note that IOP providers may not be available outside of program hours (9-12:30), so you may have to wait until the next day to speak with them outside of any scheduled appointments.
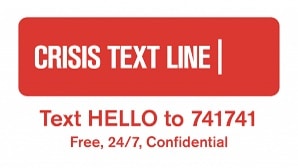
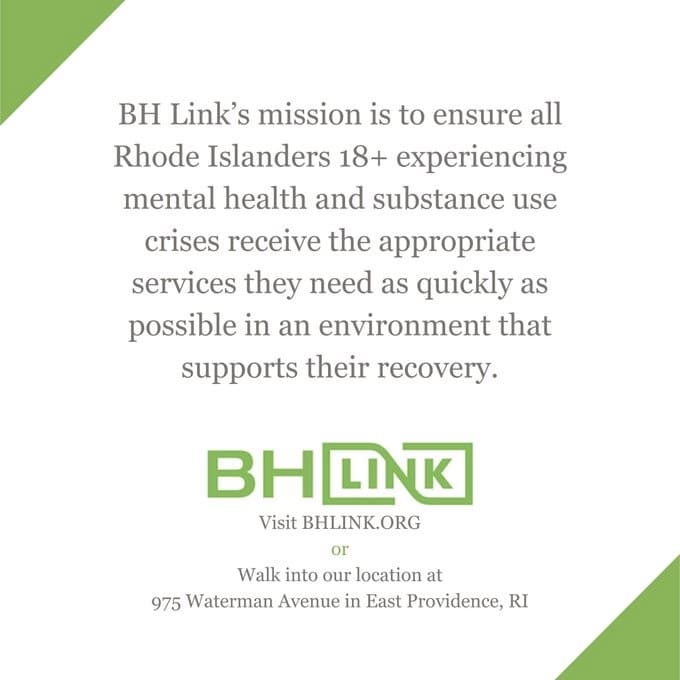
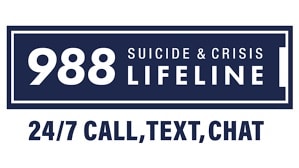
Several resources outside of IOP that are available to you 24/7 in a crisis include the National Suicide and Crisis Lifeline (call or text 988 from any phone), the Crisis Text Line (text anything to 741741), or if you are in RI, BH Link (a mental health walk in triage center located at 875 Waterman Ave, East Providence, RI; call 401-414-5465). These resources are also pictured at the bottom of this page.
If you are having an increase in suicidal thoughts and are unable to remain safe, please do not wait to speak with your treatment team. Call 911 or go to the nearest emergency room if you are not able to maintain safety at any point.